More Information
Submitted: December 13, 2021 | Approved: December 30, 2021 | Published: December 31, 2021
How to cite this article: Lombard CM, Naruns PL. Painful unilateral gynecomastia with identification of the cause of the pain: A case report. Arch Pathol Clin Res. 2021; 5: 034-036.
DOI: 10.29328/journal.apcr.1001026
Copyright License: © 2021 Lombard CM, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Gynecomastia; Unilateral; Painful; Pathogenesis; Pathology
Painful unilateral gynecomastia with identification of the cause of the pain: A case report
Charles M Lombard1* and Peter L Naruns2
and Peter L Naruns2
1Department of Pathology, El Camino Hospital Mountain View, CA 94040, USA
2Department of Surgery, El Camino Hospital Mountain View, CA 94040, USA
*Address for Correspondence: Charles M Lombard, MD, Department of Pathology GC # 431, 2500 Grant Road, El Camino Hospital Mountain View, CA 94040, USA, Email: [email protected]
A 69-year-old man presented with a one-month history of a painful mass in the right breast. Pathologic evaluation of the excision of the mass revealed a proliferation of both glandular and stromal elements consistent with gynecomastia. In addition, histologic examination revealed peripheral nerves in the deep portion of the specimen were entrapped in the proliferative changes associated with gynecomastia. It is proposed that the expansile proliferation led to compressive pressure on the nerves and caused the pain associated with gynecomastia.
Gynecomastia is a common condition afflicting males of all ages. It is estimated that 50% of adolescent males develop some degree of gynecomastia. In men older than 50 years of age as many as 65% experience some degree of gynecomastia [1]. Physiologic gynecomastia results from an imbalance of free testosterone and estradiol concentrations and can be seen within 3 age ranges: 1) neonates, 2) adolescents, and 3) aging men over the age of 50. Benign non-physiologic gynecomastia may occur at any age and there are a variety of etiologies including numerous medications, endocrine disorders, metabolic disorders, and tumor-associated gynecomastia [1]. In most cases gynecomastia is bilateral, although unilateral gynecomastia is also well known. The frequency of unilateral gynecomastia is not well described and ranges from 14% to 50% [2,3]. Pain is a common feature of gynecomastia, although the pain is most often a generalized discomfort in the hypertrophied breast tissues. Severe pain is an infrequent finding in gynecomastia. The cause of the pain in gynecomastia has never been identified.
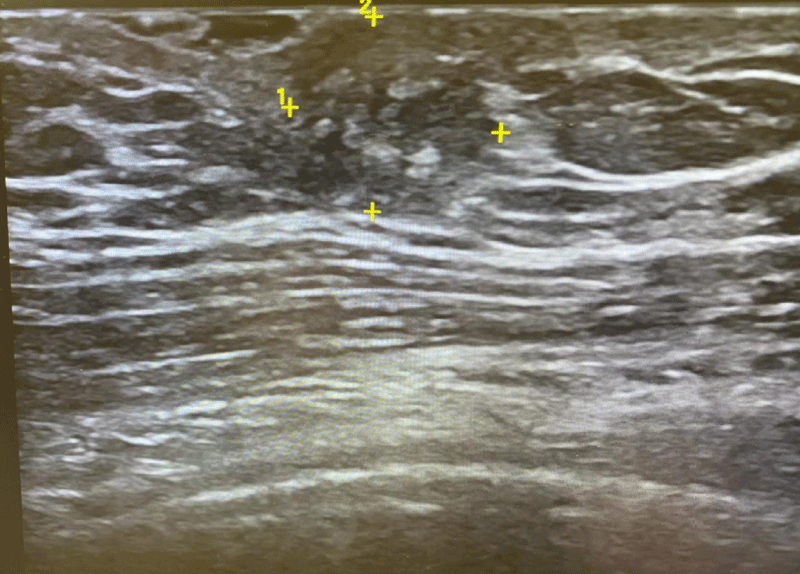
A 69-year-old man noted a painful mass in the right breast. When the patient presented for medical attention, the painful mass had been present for one month. On examination, a painful circumscribed movable nodule with a smooth surface measuring an estimated 1 cm in diameter was palpated in the inferior subareolar tissues. The nodule was exquisitely tender on palpation and the patient reported that there was also a continuous dull aching pain in the breast. The contralateral breast was unremarkable. There was no axillary lymphadenopathy. An ultrasound examination revealed a nodular hypoechoic area in the subareolar region of the breast (Figure 1). The patient’s past medical history was remarkable for severe carotid atherosclerosis requiring a carotid endarterectomy 4 years previously. The patient was also known to have severe calcific coronary artery disease. 2 years prior to presentation the patient developed polymyalgia rheumatic and had been treated with prednisone for this condition. The prednisone had been discontinued one month prior to the onset of the gynecomastia symptoms. The patient’s medications are shown in Table 1. Liver function tests, renal function tests, and thyroid function tests were unremarkable. Total and free testosterone levels were normal. Although unilateral gynecomastia was included in the differential diagnosis for this nodule, it was difficult to exclude a neoplasm of the breast and the patient was offered diagnostic needle biopsy versus excision of the mass. The patient chose excision and this was successfully completed.
Figure 1: Ultrasound of breast lesion. Ultrasound shows a hypoechoic rounded area in the subareolar tissues.
| Table 1: Patient Medications. | |||
| Drug | Dose | Frequency/Duration of treatment | Association with Gynecomastia |
| Lisinopril | 10 mg | Once a day/4 years | Rare/unlikely [5,6] |
| Aspirin | 81 mg | Once a day/4 years | No reported association [5,6] |
| Omeprazole | 20 mg | Once a day/18 months | Possible association/rare [5,6] |
| Repatha | 140 mg/ml | A subcutaneous injection every 15 days/18 months | No reported association [5,6] |
| Coenzyme Q | 200 mg | Once a day/4 years | No reported association [5,6] |
| Melatonin | 10 mg | Episodic for treatment of jet lag | Rare isolated case report/rare [7] |
| Prednisone | 50 mg/taper | Daily on a tapering schedule/ 17 months discontinued 1 month prior to the onset of gynecomastia | No reported association [5,6] |
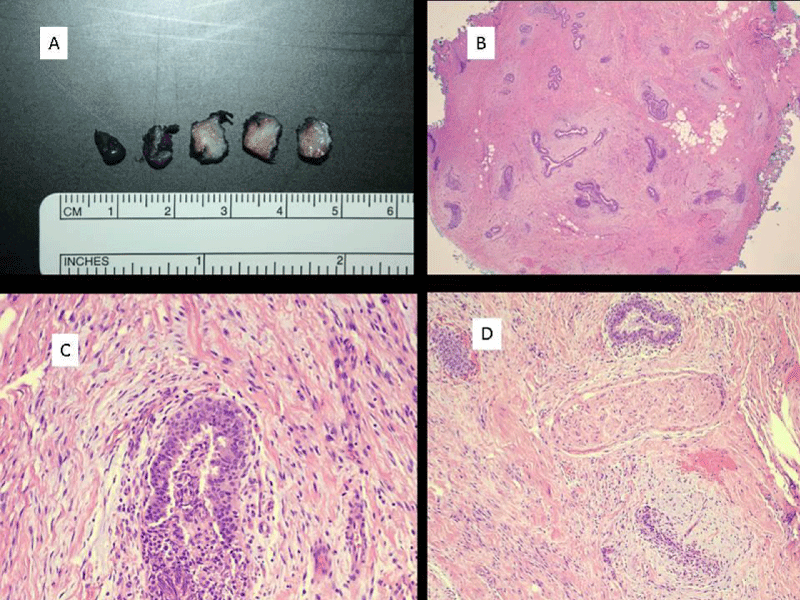
Pathologic evaluation of this specimen revealed changes characteristic of gynecomastia (Figure 2A-D). The gross specimen revealed a circumscribed area of firm edematous fibrous tissue measuring 1.5 x 0.8 x 0.7 cm. Microscopic examination revealed a proliferation of glandular and stromal elements without atypia, characteristic of gynecomastia. There was moderate edema of the stromal tissues. In the deep portion of the dissection, there were peripheral nerves identified. Some of these were intimately admixed with and entrapped in the gynecomastia-associated proliferative changes causing compression of the nerve.
Figure 2: Gross appearance of gynecomastia with a circumscribed nodule of edematous fibrous tissue. B) Low power image of gynecomastia with the proliferation of glandular and stromal elements (hematoxylin and eosin; 20 x magnification). C) Image of gynecomastia showing the epithelial proliferation without atypia and the surrounding stromal proliferation with associated stromal edema (hematoxylin and eosin, 200x magnification). D) Image showing peripheral nerve intimately admixed with gynecomastia-associated proliferation and compressed between proliferation with associated edema (hematoxylin and eosin, 100 x magnification).
In a reported series of unilateral gynecomastia [4], it was noted that none of the patients had a non-physiologic cause for their gynecomastia. In addition, the age range reported (20-42) was outside the 3 age group ranges (neonates, adolescents, and men > 50 years old) for physiologic gynecomastia. Their patients fell into the idiopathic group of gynecomastia which accounts for approximately 25% of gynecomastia patients overall. Breast pain was present in 50% of the patients with unilateral gynecomastia, however, there was only slight tenderness on palpation in this series of patients. In our pathology department, 39 cases of gynecomastia came to resection over the past 5 years.
11 (28%) were cases of unilateral gynecomastia. The presence of pain was documented in 24 patients. 13 (54%) reported pain or tenderness associated with gynecomastia. Table 2 documents the age distribution of gynecomastia, the distri-bution of unilateral and bilateral cases of gynecomastia, and the presence of pain in unilateral and bilateral gynecomastia in our patients.
| Table 2: Distribution of cases of gynecomastia for which surgery was performed at El Camino Hospital 2016-2021. | |||
| Patients operated on for gynecomastia 2016-2021 (N = 38) | |||
| Age range | ≤ 20 y | 21-49 y | ≥ 50 y |
| # patients | 10 | 24 | 5 |
| # unilateral | 3 | 5 | 2 |
| Patients in whom the presence or absence of pain was documented (N = 24) | |||
| Pain present (unilateral/bilateral) |
4 (3/1) |
7 (2/5) |
2 (2/0) |
| Pain absent | 4 (0/4) |
7 (2/5) |
0 (0/0) |
In the case we report, there was marked pain on palpation and this unusual pain, in addition to the well-circumscribed nature of the nodule raised a differential diagnosis of painful soft tissue nodules, also known to occur in the breast including angiolipoma [8], vascular leiomyoma [9], glomus tumor [10], and eccrine spiradenoma [11], in addition to the possibility of unilateral gynecomastia. On excision, the typical pathologic changes of gynecomastia including both stromal and epithelial glandular hyperplasia were identified. It was concluded that this represented idiopathic nodular gynecomastia. Because of the unusual clinical feature of marked pain on palpation, a careful examination of the tissues for possible reasons for this pain was undertaken.
Examination of the specimen revealed an area in the deep tissues with prominent peripheral nerves. Some of these nerves were intimately admixed with and entrapped in the gynecomastia-associated glandular and stromal proliferation. We postulate this proliferation with associated stromal edema led to compression of the nerve structures causing pain and exquisite, marked tenderness to palpation. Although the pain associated with gynecomastia is a common clinical feature, to our knowledge there has never been a clear and convincing cause for this pain described.
In this report, we identify what we interpret as the cause of pain in gynecomastia. Peripheral nerve was identified intimately admixed with and entrapped in areas of gynecomastia. We have postulated that compressive effects on these nerves result in painful gynecomastia.
- Dickson G. Gynecomastia. Am Fam Physician. 2012; 7: 716-722.
- Wiesman IM, Lehman JA, Parker MG, Tantri MDP, Wagner DS, et al. Gynecomastia: An outcome analysis. Ann Plast Surg. 53: 97-101. PubMed: https://pubmed.ncbi.nlm.nih.gov/15269574/
- Fagerlund A, Lewin R, Rufolo G, Elander A, Santanelli di Pompeo S, et al. Gynecomastia: A systematic review. J Plast Surg Hand Surg. 2015; 311-318. PubMed: https://pubmed.ncbi.nlm.nih.gov/26051284/
- Al-Quattan M, Hassanain J, Mahmoud S, El-Shayed A, Tashkandi M, et al. On the neglected entity of unilateral gynecomastia. An Plast Surg. 2005; 55: 255-257. PubMed: https://pubmed.ncbi.nlm.nih.gov/16106162/
- Roberto G, Melis M, Biagi C. Drug-induced gynecomastia. Focus Farmacovigilanza. 2013; 77: 2-4.
- Nuttali F, Warrier R, Gannon M. Gynecomastia and drugs: a critical evaluation of the literature. Eur J Clin Pharmacol. 2015; 71: 569-578. PubMed: https://pubmed.ncbi.nlm.nih.gov/25827472/
- De Bleecker JL, Lamont BH, Verstraete AG, Schelfhout VJ. Melatonin and painful gynecomastia. Neurology. 1999; 53: 435-436. PubMed: https://pubmed.ncbi.nlm.nih.gov/10430450/
- Branca G, Irato E, Barresi V, DeMarco M, Guccione F, et al. A rare case of male breast cavernous type angioleiomyoma. Tumori. 2014; 100: 148e-152e. PubMed: https://pubmed.ncbi.nlm.nih.gov/25296607/
- Noel JC, Van Geertruyden J, Engohan-Aloghe C. Angiolipoma of the breast in a male: a case report and review of the literature. Int J Surg Path. 2011; 19: 813-816. PubMed: https://pubmed.ncbi.nlm.nih.gov/20034977/
- Mehdi G, Siddiqui FA, Ansari HA, Mansoor T. Glomus tumor occurring in a male breast: an unusual site of presentation. J Postgrad Med. 2010; 56: 218-219. PubMed: https://pubmed.ncbi.nlm.nih.gov/20739772/
- Ghai S, Bukhanov K. Eccrine acrospiroma of breast: mammographic and ultrasound findings. Clin Radiol. 2004; 59: 1142-1144. PubMed: https://pubmed.ncbi.nlm.nih.gov/15556599/