More Information
Submitted: November 21, 2023 | Approved: December 04, 2023 | Published: December 05, 2023
How to cite this article: Mkrtumyan V, Harutyunyan T, Meliksetyan L, Mkhitaryan A, Khachatryan P. A Perplexing Case of Genito-urinary Tuberculosis in an 83-Year-Old Woman with Increased Levels of Tumor Markers: A Case Report. Arch Pathol Clin Res. 2023; 7: 028-033.
DOI: 10.29328/journal.apcr.1001038
Copyright License: © 2023 Mkrtumyan V, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Case report; Genito-urinary tuberculosis; Ovarian cancer; CA-125; Ascites
Abbreviations: CBC: Complete Blood Count; CT: Computer Tomography; EP: Extra-Pulmonary; FGTB: Female Genital Tuberculosis; GUTB: Genito-Urinary Tuberculosis; HbsAg: Hepatitis B Surface Antigen; HCV: Hepatitis C Virus; HIV: Human Immunodeficiency Virus; MSCT: Multislice Computed Tomography; PCR: Polymerase Chain Reaction; PTB: Pulmonary Tuberculosis; TB: Tuberculosis
A Perplexing Case of Genito-urinary Tuberculosis in an 83-Year-Old Woman with Increased Levels of Tumor Markers: A Case Report
Voskehat Mkrtumyan1,2, Tamara Harutyunyan1,2, Lilit Meliksetyan2* , Armen Mkhitaryan1,2 and Parandzem Khachatryan1,2
, Armen Mkhitaryan1,2 and Parandzem Khachatryan1,2
1“Histogen” Armenian-German Scientific-Practical Center of Pathology, Armenia
2Yerevan State Medical University, Armenia
*Address for Correspondence: Lilit Meliksetyan, “Histogen” Armenian-German Scientific-Practical Center of Pathology, Yerevan, Nor Aresh 9 str, Armenia, Email: [email protected]
Background: Tuberculosis (TB) is a significant global health problem, and extrapulmonary TB can present with no specific clinical or radiographic findings. Genito-urinary TB is often associated with elevated tumor markers and can be misdiagnosed as ovarian/fallopian tube carcinomas, especially in elderly female patients, as genitourinary TB commonly affects women of reproductive age.
Objective: We present a rare case of genito-urinary TB in an elderly female patient who was initially misdiagnosed with ovarian cancer with metastasis.
Case presentation: An 83-year-old woman with a medical history of diabetes and hypertension presented with complaints of abdominal distension. Diagnostic imaging revealed lesions in the ovaries and omentum and tumor markers were elevated, leading to a suspicion of ovarian cancer with metastases to the omentum. The patient underwent a diagnostic laparotomy and surgical removal of ovaries, fallopian tubes, and the lesion of the greater omentum. However, no malignancy was found during the morphological evaluation. Further histopathological examination confirmed the final diagnosis of genito-urinary tuberculosis, and the patient received anti-TB drugs. The postoperative period was uneventful, and tumor marker levels decreased.
Conclusion: As the clinical presentation of genito-urinary TB can mimic ovarian cancer, a histopathological examination should be performed for differential diagnosis, thereby reducing the possibility of inaccurate treatment. This case report highlights the importance of considering genito-urinary TB as a differential diagnosis in elderly female patients presenting with elevated tumor markers, abdominal distension, and suspected genital malignancy. It is crucial to carefully evaluate these cases and explore the possibility of genital TB as an alternative diagnosis, given the overlapping clinical presentation. This highlights the importance of a comprehensive diagnostic approach that includes considering TB in addition to malignancy, even in the context of elderly female patients.
Tuberculosis (TB) is a global health concern, with about a quarter of the world’s population estimated to have been infected with TB [1]. Armenia recorded an incidence of 27 tuberculosis cases per 100,000 people in 2021. Throughout the period from 2005 to 2021, there was an average annual decrease of 4.63% in tuberculosis incidence [2]. Genitourinary tuberculosis (GUTB) is a secondary manifestation of pulmonary TB caused by Mycobacterium tuberculosis bacilli. GUTB can cause fallopian tube blockage and is a leading cause of female infertility, particularly in underdeveloped countries [3]. Extra-pulmonary tuberculosis (EPTB) can have a variety of manifestations, including menstrual dysfunctions (10% - 40%), infertility (43% - 74%), systemic symptoms such as fever, weight loss, malaise, abdominal and pelvic pain (25% - 50%), fullness, tenderness, ascites, and various clinical signs such as bleeding, leucorrhoea, and pyometra [4]. However, these signs are often mistaken for other conditions such as gynecological malignancies, appendicitis, ovarian cysts, extra uterine pregnancy, and chronic pelvic inflammatory disease. In postmenopausal women, GUTB often presents with radiographic and laboratory findings similar to those of endometrial or ovarian cancer [5,6]. Furthermore, it can be challenging to differentiate between GUTB and genital malignancies radiologically, as both conditions can present with a pelvic mass, ascites, thickened peritoneum, and omental involvements [5,7]. Additionally, some cases of GUTB may present with elevated tumor markers such as cancer antigen 125 (CA-125) [7]. Misdiagnosis may lead to unnecessary radical surgical treatment [8]. Here, we report a rare case of an elderly female patient with GUTB involving the greater omentum and highlight the differential diagnosis between ovarian cancer and GUTB, with reference to current medical literature.
An 83-year-old female presented to the hospital with a 3-month history of progressive abdominal distension. She had a medical history of diabetes mellitus and hypertension and was taking daily medications for blood sugar and blood pressure control. There was no history of infectious diseases, and her family history was unremarkable. She had attained menopause 30 years ago. On examination, she was afebrile with a blood pressure of 135/85 mmHg, a heart rate of 101 beats per minute, and a respiratory rate of 15 breaths per minute. She appeared pale, and there was no jaundice. Abdominal percussion revealed normal bowel sounds and positive shifting dullness due to ascites. No hepatosplenomegaly was observed.
Abdominal and pelvic ultrasound showed no hepatosplenomegaly but revealed a significant amount of intraperitoneal fluid with multiple septations without vascularity as confirmed by a Color Doppler study. An interstitial myometrial nodule measuring 7mm was also noted in the uterus. Laboratory investigations including complete blood count (CBC) and biochemical tests are presented in Table 1. Human Immunodeficiency Virus (HIV), Hepatitis C Virus (HCV), and Hepatitis B surface antigen (HBsAg) tests were negative. Liver function tests were within normal limits, thus liver pathology was excluded as the most common cause of ascites. Based on these findings, an ovarian malignant tumor was suspected, and tumor markers were measured. The results of the tests are presented in Table 2.
| Table 1: Complete blood count and biochemical test results. | ||
| Variable, range | Reference, adult | Patients’ data |
| Hemoglobin (g/l) | 115-145 | 100 |
| Hematocrit (%) | 35-47 | 31 |
| Red blood cells (x1012/ml) | 3.7-4.7 | 3.8 |
| Mean corpuscular volume (MCV, fl) | 80-95 | 79.9 |
| Mean hemoglobin concentration (MCH, pg) | 26-34 | 25.8 |
| Platelets (x109/L) | 150-400 | 616 |
| White blood cells (x109/L) | 4.0-10.0 | 6.8 |
Granulocytes (%)
|
- 1-6 42-72 |
- 1 70 |
| Eosinophils (%) | 0.5-5 | 0 |
| Basophils (%) | 0-1 | 0 |
| Lymphocytes (%) | 19-37 | 20 |
| Monocytes (%) | 3-11 | 9 |
| Plasma cells (%) | 0 | 0 |
| Erythrocyte sedimentation rate (ESR, mm/hour) | 2-15 | 71 |
| Glucose (mmol/l) | 3.3-5.5 | 9.81 |
| Urea (mmol/l) | 1.7-8.3 | 12.8 |
| Creatinine (µmol/l) | 44-80 | 102.5 |
| Total protein (g/l) | 66-87 | 87.6 |
| Total bilirubin (µmol/l) | 2.55-20.5 | 6.6 |
| Direct bilirubin (µmol/l) | 2-5.4 | 2.8 |
| ALT (U/L) | 33 | 7 |
| AST (U/L) | 32 | 13.8 |
| C reactive protein (mg/l) | < 5 | 144.6 |
| Rheumatoid factor (IU/ml) | < 14 | negative |
| Antistreptolysin O (U/ml) | < 200 | negative |
| Rose Bengal | negative | negative |
| Fibrinogen (mg/dl) | 200-400 | 327 |
| Prothrombin index (%) | 80-100 | 65 |
| Prothrombin time (PT, sec.) | 12-16 | 15.8 |
| INR | 1-2 | 1.38 |
| * - ranges are given by the entire laboratory for adult females. | ||
| Table 2: Tumor markers test result. | ||
| Variable, range | Reference, adult | Patients’ data |
| ROMA (%) | 0-29 | 87.271 |
| Human epididymis protein 4 (pmol/L) | Premenopausal, < 70 Postmenopausal, < 140 |
271.5 |
| CA 125 (Uml) | < 35 | 304.9 |
A multislice computed tomography (MSCT) of the chest, abdomen, and pelvis revealed mediastinal lymphadenopathy, large ascites, lesions in both ovaries and greater omentum, a cyst of the left kidney, and hiatal hernia. No significant lesions or foci indicating primary lung pathology, such as tumors or tuberculosis, were detected during the examination of the lungs. The ovaries were diffusely changed, and the conclusion suggested that the findings may be characteristic of ovarian cancer. Hence, before the surgery, paracentesis and cytological examinations were performed to exclude the possibility of cancer.
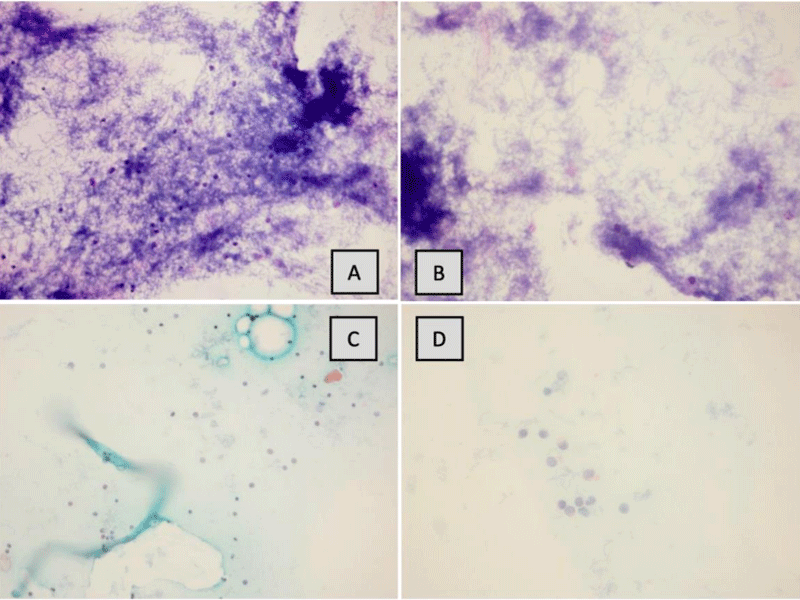
Cytological examination
A sample of 300 mL yellowish fluid was collected, and Papanicolaou (PAP) staining and Diff-Quick staining cytological slides were prepared. On microscopic examination of the specimen, a large number of bacilli, spores, and lymphocytes were present, and no neoplastic cells were found (Figure 1).
Figure 1: A and B – DQ staining, 5× and 10× magnification. C and D – PAP, 5× and 10× magnification. Similar cytologic findings described: a large number of bacilli, spores, and lymphocytes. Neoplastic cells were not detected.
As the final diagnosis was still uncertain, the surgeon recommended a diagnostic laparotomy, which the patient agreed to undergo. However, due to financial constraints, the patient declined to have a frozen section biopsy. Taking into consideration that frozen section biopsy is not mandatory according to our country’s surgical protocol and the patient’s age, where fertility preservation was not a concern, it was decided not to proceed with the biopsy. Consequently, during the laparotomy, bilateral adnexectomy and resection of the metastatic foci from the omentum were performed, and the resected specimens were sent for histopathological examination.
Histopathological examination
On gross examination, both ovaries and fallopian tubes were not enlarged. The right and left ovaries measured 2.7×1.5×0.8 and 2.5×1.5×0.8 cm³, respectively, while the fallopian tubes were 5.5 and 6.0 cm in length. No abnormal masses were found during sectioning. In the sample of the greater omentum, a lesion with firm consistency and 1.5 cm in diameter was described.
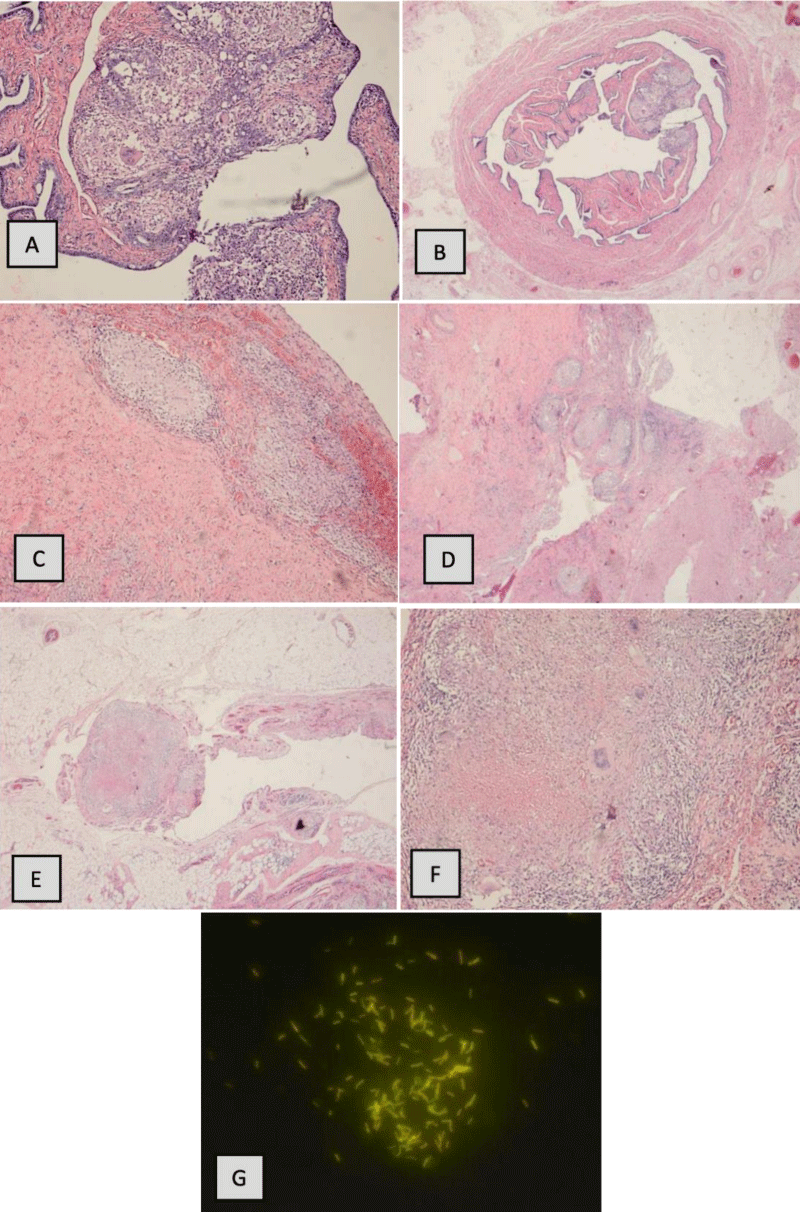
The slides were stained with Hematoxylin and Eosin (H&E), and the microscopic examination revealed numerous caseating granulomas composed of epithelioid cells. A number of multinucleated giant cells were observed. Neoplastic cells were not found in any of the sections. Additionally, auramine-rhodamine staining was done, and the acid-fast bacilli were detected under microscopy.
The summary of the histopathological examination was bilateral granulomatous salpingoophoritis with granulomatous omentitis, the results were consistent with GUTB (Figure 2).
Figure 2: A and B – H&E staining of the fallopian tube, 5× and 10× magnification. Giant cells and granulomas are seen. C and D – H&E staining of ovaries, 5× and 10× magnification. Similar histologic findings are described in the fallopian tube. E and F- H&E staining of omentum, 5× and 10× magnification, granulomas are evident. G- auramine-rhodamine stain and acid-fast bacilli are revealed.
Subsequently, the patient was referred to the “National Center of Pulmonology” for further evaluation and management. The diagnosis of GUTB was confirmed, and she was initiated on anti-tuberculosis treatment. Throughout the one-year follow-up period, tumor marker levels returned to normal, indicating a positive outcome. Additionally, no postoperative complications were observed during this time.
The prevalence of GUTB is often underestimated since the majority of affected patients are asymptomatic. GUTB is typically diagnosed in females of reproductive age during evaluation for infertility, as it can cause inflammation of the fallopian tubes, uterus, and ovaries [9,10]. While approximately 11% of GUTB cases are in the postmenopausal age group [11], it can also mimic other pelvic disorders such as genital malignancies, which can make diagnosis difficult. This is especially true in older adults where clinical and radiological findings may present as ascites, abdominal distension, weight loss, and elevation of tumor markers [8,9,12]. Thus, the diagnosis of GUTB should include a combination of multiple diagnostic tests [12,13]. A thorough evaluation may involve Computed Tomography (CT), ultrasonography, histopathological examination, and checking CA-125 levels to differentiate from mimicking diseases [14]. The characteristic tubercular changes in fallopian tubes and uterus are best detected during hysterosalpingogram and ultrasound, while CT should be chosen in cases with the involvement of ovaries and peritoneum [12].
Limited data is available regarding the potential elevation of CA-125 levels in tuberculosis cases. However, the authors of the study reported that CA-125 levels have shown utility in diagnosing GUTB, particularly in patients with peritoneal tuberculosis. In such cases, CA-125 is considered a marker with an average sensitivity of 83.33% and specificity of 50%. [14,15]. However, elevated CA-125 levels are commonly found in patients with ovarian malignancies, which can lead to misdiagnosis. CA-125 levels can also be increased in many other conditions such as during menstruation, the first trimester of pregnancy, the postpartum period, endometriosis, and pelvic inflammatory disease [16,17]. Although the presence of pelvic lesions associated with omental involvements, ascites, and high CA-125 levels usually refers to pelvic malignancies, differentiation with GUTB should be considered.
Human epididymis protein 4 (HE4) is primarily associated with elevated levels in epithelial ovarian cancers, endometrial carcinomas, and lung cancer. HE4 has shown potential as a diagnostic tool in these malignancies, contributing to the identification and monitoring of these specific types of cancer. Elevated HE4 has shown potential as a diagnostic biomarker for pulmonary tuberculosis. A study evaluating HE4 levels in TB, chronic bronchitis, and healthy control subjects found significantly higher HE4 concentrations in pulmonary TB patients compared to chronic bronchitis and healthy controls. Additionally, higher HE4 levels were observed in advanced pulmonary TB (PTB) cases compared to mild to moderate TB. These findings suggest that elevated serum HE4 levels could serve as a useful biomarker for diagnosing PTB and assessing disease severity [18].
Histopathological examination is another crucial step in confirming a diagnosis of GUTB [12]. The diagnosis of tuberculosis is characterized by specific findings such as caseous granulomas surrounded by epithelioid cells, lymphocytes, plasma cells, and giant cells [19]. While Acid Fast Bacilli staining is an inexpensive test with variable sensitivity, it may support the definitive diagnosis [14,20]. The best method of sampling is ultrasound-guided biopsy, which is a minimally invasive procedure with high diagnostic accuracy [20,21].
The polymerase chain reaction (PCR) is another diagnostic tool used for the rapid diagnosis of TB, which can also detect the genotype. PCR is a simple, reliable, low-cost, fast, and accurate test [22,23]. However, the differentiation between active and latent infections cannot be detected using the PCR method [14].
The treatment for GUTB involves a combination of anti-TB drugs. Isoniazid, Ethambutol, and Pyrazinamide are the drugs of choice for the intensive phase, while Isoniazid, Rifampicin, and Ethambutol are used in the continuation phase. Surgical treatment may also be suggested in patients with tubo-ovarian mass, abscess, and/or adhesions [14].
Our case report highlights the importance of considering GUTB as a differential diagnosis in postmenopausal women with clinical and radiological findings mimicking genital malignancies. The histopathological examination remains the gold standard for diagnosis confirmation, and a combination of diagnostic tests may be required to achieve an accurate diagnosis. We believe that raising awareness of GUTB in elderly women can lead to early diagnosis and appropriate treatment, thus preventing further complications. Therefore, it is crucial to consider GUTB as a possible diagnosis in postmenopausal women with suspicious symptoms, even in low TB prevalence areas.
Declarations
Acknowledgement: Published with written consent of the patient, authors, and medical personnel involved.
Availability of data and material: ‘Histogen’ Armenian-German Scientific-Practical Center of Pathology provided the data, specimen samples, and report of investigations.
Ethical approval: We confirm that explicit written consent to publish the results has been received from the described patient.
Consent: Written informed consent was obtained from the patients for the publication of this case report and any accompanying images. A copy of the written consent is available for review to the editor-in-chief of this journal.
Author contributions: P.S.K: Validation, reviewing, editing the manuscript and Supervision; V.R.M: Project Administration, Writing, reviewing manuscript; T.A.H: Data Curation, Investigation; A.G.M: Conceptualizing and Supervision.
- Global tuberculosis report 2022. World Health Organization. https://www.who.int/teams/global-tuberculosis-programme/tb-reports/global-tuberculosis-report-2022
- Armenia Incidence of Tuberculosis, 1960-2022 - Knoema.com. Knoema, knoema.com/atlas/Armenia/topics/Health/Risk-factors/Incidence-of-tuberculosis. Accessed 23 June 2023.
- Kesharwani H, Mohammad S, Pathak P. Tuberculosis in the Female Genital Tract. Cureus. 2022 Sep 2;14(9):e28708. doi: 10.7759/cureus.28708. PMID: 36204039; PMCID: PMC9527183.
- Zajaczkowski T. Genitourinary tuberculosis: historical and basic science review: past and present. Cent European J Urol. 2012;65(4):182-7. doi: 10.5173/ceju.2012.04.art1. Epub 2012 Dec 11. PMID: 24578959; PMCID: PMC3921817.
- Shim SW, Shin SH, Kwon WJ, Jeong YK, Lee JH. CT Differentiation of Female Peritoneal Tuberculosis and Peritoneal Carcinomatosis From Normal-Sized Ovarian Cancer. J Comput Assist Tomogr. 2017 Jan;41(1):32-38. doi: 10.1097/RCT.0000000000000446. PMID: 27636249.
- Diop AD, Fontarensky M, Montoriol PF, Da Ines D. CT imaging of peritoneal carcinomatosis and its mimics. Diagn Interv Imaging. 2014 Sep;95(9):861-72. doi: 10.1016/j.diii.2014.02.009. Epub 2014 Mar 14. PMID: 24631039.
- Chien JC, Fang CL, Chan WP. Peritoneal tuberculosis with elevated CA-125 mimicking ovarian cancer with carcinomatosis peritonei: Crucial CT findings. EXCLI J. 2016 Nov 16;15:711-715. doi: 10.17179/excli2016-625. PMID: 28337102; PMCID: PMC5318682.
- Efared B, Sidibé IS, Erregad F, Hammas N, Chbani L, El Fatemi H. Female genital tuberculosis: a clinicopathological report of 13 cases. J Surg Case Rep. 2019 Mar 23;2019(3):rjz083. doi: 10.1093/jscr/rjz083. PMID: 30937159; PMCID: PMC6431246.
- Neonakis IK, Spandidos DA, Petinaki E. Female genital tuberculosis: a review. Scand J Infect Dis. 2011 Aug;43(8):564-72. doi: 10.3109/00365548.2011.568523. Epub 2011 Mar 28. PMID: 21438789.
- Grace GA, Devaleenal DB, Natrajan M. Genital tuberculosis in females. Indian J Med Res. 2017 Apr;145(4):425-436. doi: 10.4103/ijmr.IJMR_1550_15. PMID: 28862174; PMCID: PMC5663156.
- Ahmed S, Shaha DR, Begum P, Akter T. Female genital tuberculosis. Faridpur Medical College Journal. 2018; 13(1):53-5.
- Aggarwal A, Das CJ, Manchanda S. Imaging Spectrum of Female Genital Tuberculosis: A Comprehensive Review. Curr Probl Diagn Radiol. 2022 Jul-Aug;51(4):617-627. doi: 10.1067/j.cpradiol.2021.06.014. Epub 2021 Jul 6. PMID: 34304946.
- Dahiya B, Kamra E, Alam D, Chauhan M, Mehta PK. Insight into diagnosis of female genital tuberculosis. Expert Rev Mol Diagn. 2022 Jun;22(6):625-642. doi: 10.1080/14737159.2022.2016395. Epub 2022 Jan 10. PMID: 34882522.
- Abbas S, Shams A, Rehman S, Akhtar K, Ovarian tuberculosis-A rare case report. IP J Diagn Pathol Oncol. 2022;7(2):116-118
- Hasanzadeh M, Naderi HR, Hoshyar AH, Shabane S, Shahidsales S. Female genital tract tuberculosis presenting as ovarian cancer. J Res Med Sci. 2014 Feb;19(2):184-9. PMID: 24778675; PMCID: PMC3999607.
- Smiti S, Rajagopal K. CT mimics of peritoneal carcinomatosis. Indian J Radiol Imaging. 2010 Feb;20(1):58-62. doi: 10.4103/0971-3026.59757. PMID: 20351997; PMCID: PMC2844752.
- Maheshwari A, Gupta S, Rai S, Rekhi B, Kelkar R, Shylasree TS, Menon S, Deodhar K, Thakur M, Das U, Gupta S, Tandon S. Clinical and Laboratory Characteristics of Patients with Peritoneal Tuberculosis Mimicking Advanced Ovarian Cancer. South Asian J Cancer. 2021 Apr;10(2):102-106. doi: 10.1055/s-0041-1736030. Epub 2021 Sep 30. PMID: 34604126; PMCID: PMC8483894.
- Li L, Yao Y, Liang J, Zhan X, Wang F, Yue C, Wu BQ, Hu S, Liu M, Wan J, Luo J. Serum human epididymis protein 4 concentrations are associated with severity of patients with pulmonary tuberculosis. Clin Chim Acta. 2020 Mar;502:255-260. doi: 10.1016/j.cca.2019.11.009. Epub 2019 Nov 12. PMID: 31730821.
- Thangappah RB, Paramasivan CN, Narayanan S. Evaluating PCR, culture & histopathology in the diagnosis of female genital tuberculosis. Indian J Med Res. 2011 Jul;134(1):40-6. PMID: 21808133; PMCID: PMC3171916.
- Akhtar N, Hayat Z, Nazim F. Genital Tuberculosis Mimicking Carcinoma Ovary: Can Ultrasound Guided Biopsy Be A Resolution! J Ayub Med Coll Abbottabad. 2017 Jul-Sep;29(3):496-498. PMID: 29076692.
- Wang Y, Shao R, He C, Chen L. Emerging progress on diagnosis and treatment of female genital tuberculosis. J Int Med Res. 2021 May;49(5):3000605211014999. doi: 10.1177/03000605211014999. PMID: 33983063; PMCID: PMC8127763.
- Bhanothu V, Venkatesan V. Conventional polymerase chain reaction and amplification refractory mutation system-multi-gene/ multi-primer PCR in the diagnosis of female genital tuberculosis. Arch Microbiol. 2019 Apr;201(3):267-281. doi: 10.1007/s00203-019-01631-1. Epub 2019 Feb 20. PMID: 30788519.
- Chopra S, Sharma S, Sharma K, Gupta N, Sharma A, Dhaliwal LK, Rajvanshi A, Sharma M. Evaluation of Multiplex PCR for Rapid Diagnosis of Female Genital Tuberculosis. J Assoc Physicians India. 2019 Dec;67(12):21-24. PMID: 31801325.