More Information
Submitted: July 08, 2023 | Approved: July 22, 2023 | Published: July 24, 2023
How to cite this article: Sharma P, Tahlan A, Palta A, Gupta M. Impact of COVID-19 on Laboratory Health Staff in an Indian Tertiary Care Hospital. Arch Pathol Clin Res. 2023; 7: 001-006.
DOI: 10.29328/journal.apcr.1001034
Copyright License: © 2023 Sharma P, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: COVID-19; Laboratory health workers; Questionnaire; Coping scoring system; General health questionnaire level
Impact of COVID-19 on Laboratory Health Staff in an Indian Tertiary Care Hospital
Pooja Sharma1, Anita Tahlan2*, Anshu Palta2 and Monica Gupta2
1Senior Resident, Department of Pathology, Government Medical College and Hospital, Chandigarh, 160032, India
2Professor, Department of Pathology, Government Medical College and Hospital, Chandigarh, 160032, India
*Address for Correspondence: Dr. Anita Tahlan, MD, Professor, Department of Pathology, Government Medical College and Hospital, Chandigarh, 160032, India, Email: [email protected]
Background: The COVID-19 pandemic has resulted in significant burdens globally. Healthcare workers (HCWs), at the heart of the unparalleled crisis of COVID-19, face challenges treating patients and doing testing for COVID-19: reducing the spread of infection; developing suitable short-term strategies; and formulating long-term plans. We aimed to assess the psychological impact of COVID-19 on Laboratory health staff.
Material and methods: Between February - March 2021, 72 laboratory staff workers of a tertiary care teaching hospital were invited to fill out a questionnaire regarding concerns and worries about the novel coronavirus pandemic, along with a coping scoring system and General health questionnaire level (GHQ-12) survey.
Results: Out of 72 laboratory health staff who completed the survey questionnaire, 10 were faculty members, 17 were residents (including senior residents, junior residents, and demonstrators), 39 were lab technicians, followed by 4 were attendants and 2 were data operators. Laboratory staff workers with an age group range from 30 years - 60 years had a higher level of depression symptoms than respondents with 20 years - 29 years of age. Similarly, the symptoms of anxiety were noted to be significantly higher among female respondents and respondents with age >30yrs. The most frequent concern was transmitting the infection to family than to themselves only. A considerable number of laboratory staff workers utilized online psychological resources to deal with their psychological distress.
Conclusion: The findings of this survey recognize the various problems faced by laboratory health workers during the period of COVID-19 which affect their working ability. Therefore, in the future, we have to implement such strategies that enhance the performance of laboratory workers, boost their energy level, and encourage them to take care of themselves, in times of such crisis.
There is a new public health crisis threatening the world with the emergence and spread of the 2019 novel coronavirus (2019-nCoV) or the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) [1,2]. After causing significant morbidity and mortality in China, by February 2020, COVID-19 had spread to numerous other countries [1-3]. Health and Social Care Workers (HSCWs) continue to play a vital role in our response to the COVID-19 pandemic [4]. Health and Social Care Workers (HSCWs) have carried a heavy burden during the COVID-19 crisis and, in the challenge to control the virus, have directly faced its consequences [4,5].
The role of laboratory medicine in times of an infectious disease outbreak has been widely established [6]. Literature review contributes to the fact that the etiological diagnosis of COVID-19, was not possible without laboratory services, either by detecting the pathogen in biological samples with reverse transcriptase-polymerase chain reaction (RT-PCR), or by quantifying antibody response immunologically [7]. COVID-19 posed a significant threat by presenting several challenges. These included inadequate availability of human resources, transportation issues, lack of Personal Protective Equipment (PPE), delayed delivery and sometimes unavailability of essential supplies, deteriorating revenue targets, health-related problems of the employees, and most importantly, a growing fear and anxiety amongst the frontline staff. Despite all these challenges, the laboratory professionals provided the best possible diagnostic support to the clinicians in this public health crisis [8].
This survey aimed to analyze the lab professionals’ perspectives serving at the pathology laboratory, in terms of the challenges, financial implications, fears, motivation level, and satisfaction from organizational processes and policies adopted, amid the COVID-19 crisis.
This study utilized a cross-sectional survey design and was conducted in the Department of Pathology and Laboratory Medicine, from February 2021 – March 2021, when there was no spread of the pandemic in our hospital. The survey was administered online via the google docs survey tool, to elicit information about social and financial well-being, stress due to the COVID-19 pandemic, and satisfaction with organizational policies and practices among medical laboratory professionals.
A team designed the survey questionnaire with discussions on COVID-19 and its impact on the personal and professional lives of laboratorians. With the laboratory staff’s inherent time constraints in mind, the survey was structured in such a way that it did not consume much time of a participant’s time. It consisted of various items grouped into three sections. The initial section consisted of demographics with a description of their role in the lab, experience, and educational level. The next two sections included measuring the effective and ineffective ways of coping with a stressful life event and assessing the psychological strains and mental health. These were more oriented toward the social, mental, and financial impact of COVID-19 on the employees alongside their satisfaction and awareness of organizational policies, practices, and measures taken amid the pandemic emergency, adequacy of resources, and extent of training. The questionnaire was then self-administered using google docs online. An email requesting participation was sent to all the full-time lab professionals including faculty, residents, technologists, data operators, and housekeeping staff serving the Pathology department (n = 72).
Participation in the survey was completely voluntary and any person can opt out and withdraw by not submitting the answers. To ensure confidentiality any personal details including email ids that might lead to identification of the personnel were not acquired as part of the survey.
This survey presents data from 72 lab professionals at varying stages in their professional careers in the department of pathology who completed the survey questionnaire.
Demographic characteristics
Most of the respondents were in the 3rd-4th decade of life. Respondents were predominantly female in the ratio of male to female was 1:7. Out of 72 laboratory staff workers, 10 were faculty members, 17 were residents (including senior residents, junior residents, and demonstrators), 39 lab technicians, 4 were attendants and 2 were data operators as shown in Table 1. Laboratory staff workers with an age group range from 30 years - 60 years had a higher level of depression symptoms than respondents with 20 years - 29 years of age. Similarly, the symptoms of anxiety were noted to be significantly higher among female respondents and respondents with age >30yrs.
| Table1: Demographic characteristics. | ||
| Variables | N (%age) | |
| Gender | Male | 9 (12.5%) |
| Female | 63 (87.5%) | |
| Designation | Faculty | 10 (13.8%) |
| Residents | 17 (23.6%) | |
| Technicians | 39 (54.2%) | |
| Data operators | 2 (2.8%) | |
| Lab attendants | 4 (5.6%) | |
General questionnaire and satisfaction from organizational processes and policies adopted, amid the COVID-19 crisis.
The general questionnaire included various questions related to the impact of COVID-19 on the physical health of laboratory staff.
Infectivity rate (Did you come positive for COVID-19 at any time?)
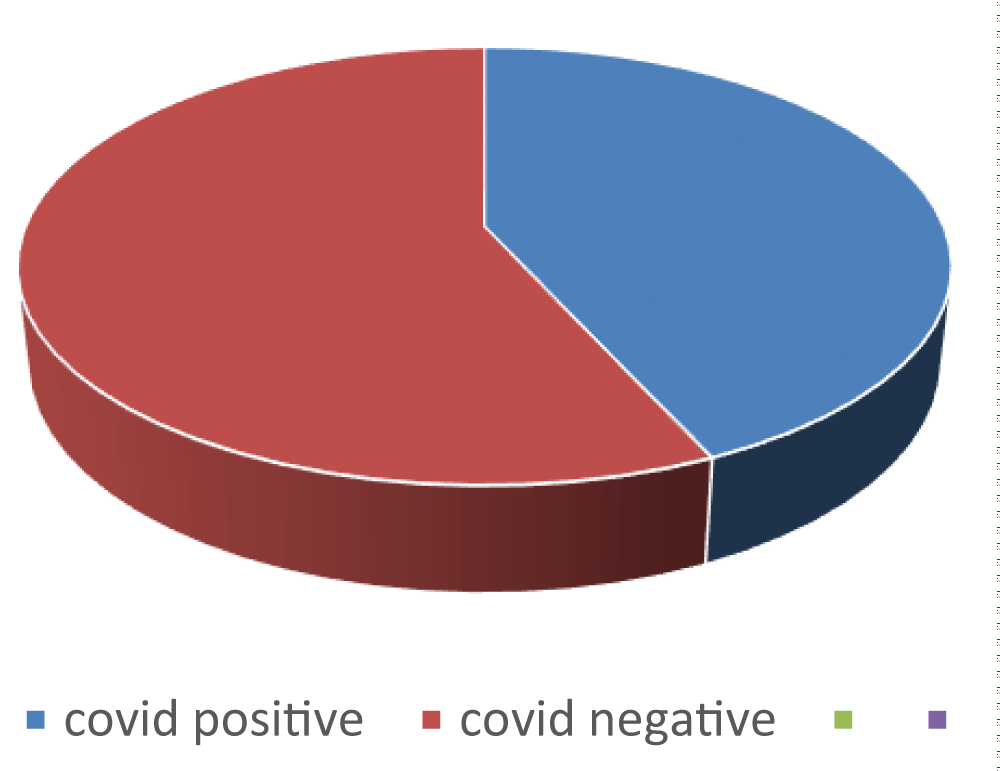
76.3% (n = 55) of lab workers were directly involved in COVID-19 patient services. 44.4% (n = 32) came positive in 1st wave of corona before the survey and 55.6% (n = 40) never came out to be positive as shown in Figure 1.
Figure 1: Infectivity rate of COVID in lab workers.
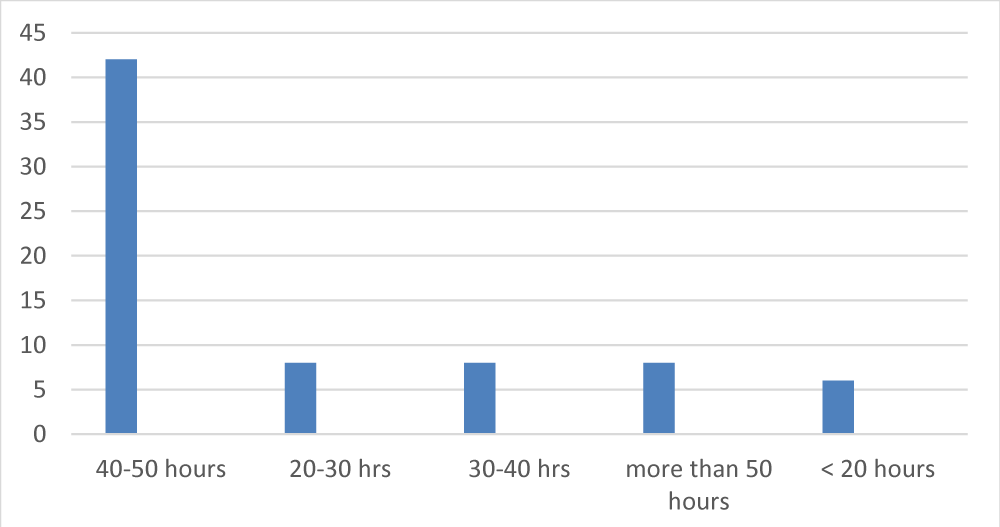
Working hours
Working hours were also affected by COVID-19. As working hours were increased and categorized in different ranges according to per week. 59% (n = 42) lab workers worked for 40 hours - 50 hours per week, 11% (n = 8) lab workers each were working for 20 hrs - 30 hrs, 30 hrs - 40 hrs, and more than 50 hours followed by 8% (n = 6) were working for less than 20 hours as shown in Figure 2.
Figure 2: Working hours spent by lab workers in COVID times.
Practices in a laboratory have changed during the COVID-19 pandemic
COVID-19 changed the way of working laboratory health staff work. 49% (n = 35) of lab workers agreed that their way of working has been changed around 30% - 50%. Each of the 18% (n = 13) of lab workers accepted that lab practices have been changed to around 50% - 80% and less than 30%. According to 10% (n = 7) of lab staff, practices have changed more than 80% followed by 6% (n = 4) of staff workers who agreed that no change has been done in laboratory practices during COVID-19 as shown in Table 2.
| Table 2: Timings in a laboratory have changed during the COVID-19 pandemic. | |
| Duration of working hours changed | Total no. of members |
| <30% | 18% (n = 13) |
| 30% - 50% | 49% (n = 35) |
| 50% - 80% | 18% (n = 13) |
| >80% | 10% (n = 7) |
| No change | 6% (n = 4) |
Apprehensive about your safety
The questions inquired how participants felt at all about their safeties which were documented as follows - apprehensive, very apprehensive, extremely apprehensive, and not apprehensive. 27 (38%) were apprehensive, 22 (31%) were very apprehensive followed by 15 (21%) somewhat apprehensive, 7 (10%) extremely apprehensive and 1 (1%) was not apprehensive at all. One of the staff believed that their prior safety training and education were lacking to effectively confront this situation.
Does your hospital have a policy to test healthcare workers if accidentally exposed to COVID-19 patients at the workplace?
Eighty-seven percent (n = 63) of survey participants were overall satisfied with the measures adopted by the institution to tackle the crisis. But 13% (n = 9) of staff members felt that the hospital premises didn’t have a policy for exposed health workers as shown in Table 3.
| Table 3: The hospital has the policy to test healthcare workers if accidentally exposed to COVID-19 patients at the workplace. | |
| Hospital measures | Total no. of members |
| Satisfied with the measures | 87% (n = 63) |
| Not satisfied with the measures | 13% (n = 9) |
Were you provided with adequate safety equipment (gloves, aprons, caps, PPE, etc)
Around 67% (n = 48) lab workers felt that there was sufficient and timely provision of personal protective equipment followed by 32% (n = 23) lab workers who felt that more than adequate kits were provided, and 1% (n = 1) felt that there was no sufficient safety equipment provided by hospital administration.
What is the policy of post-test quarantine for healthcare workers in case of exposure at your workplace? Please specify
The responses were documented as 36% (n = 26) lab workers agreed that they were quarantined at home after contact with a positive patient, 31% (n = 22) were quarantined at home as COVID positive, 13% (n = 9) didn’t know the status, 19% (n = 14) were quarantined at the hospital after contact with the positive patient and 1% (n = 1) was quarantined at the hospital as COVID positive.
If quarantined at home/hospital, how did you utilize your time? Check all that apply
Approximately 42% (n = 30) of lab workers agreed that they utilized their time on social media, 14% (n = 10) of lab staff read books, 7% (n = 5) each enjoyed the music and spent time with family, 6% (n = 4) utilized time doing yoga and 32% (n = 23) spent time by utilizing all above activities.
The psychological toll on healthcare workers
The psychological toll included two questionnaire levels, one was a coping level and the other was a general health questionnaire.
Coping level: This questionnaire is for measuring the effective and ineffective ways of coping with a stressful life event. To ensure staff’s sense of meaning and engagement indicators of stress included in the survey were an inquiry regarding their coping level amidst the COVID-19 times and the impact of declining workload on their routine activities. More than half i.e. 80% of the laboratorians agreed that they feel a low level of energy and enthusiasm while coming to work, which they had before these rough times. They have been turning to work or other activities to take their minds off things. The coping level was measured as a healthy way and the unhealthy way in which the total survey questionnaire was 28 and they scored 1 - 4. The healthy way was scored 1-2 and the unhealthy way was scored 3 - 4. Seventy percent (n = 51) of laboratory workers fell under unhealthy way of coping and 30% (n = 21) of staff fell under healthy way of coping (Table 4).
| Table 4: Percentage of members cope in different ways. | ||
| cope in healthy ways | use unhealthy ways of coping | |
| Scores (1 - 4) | 1 - 2 scores | 3 - 4 scores |
| Total members | 21 (30%) | 51 (70%) |
General health questionnaire level (GHQ-12): It included 12 questions that assessed the psychological strains and mental health. They ranged from 1-4 included - better than usual, same as usual, less than usual, and much less than usual. For GHQ-12 cut-off is 2/3, that is no psychological stress at 2 or below and a score of 3 or above indicates concern. For those scoring 2 or below the statement might be Wonderful, they were doing very well. Those scoring 3 and above can be asked to relax. Sixty-eight percent (n = 49) of laboratory workers scored 3 or above, so there was a need for concern and asked to relax while 32% (n = 23) workers scored 2 or below as shown in Table 5. The most frequent concern was transmitting the infection to family than to themselves only.
| Table 5: General health questionnaire level (GHQ-12). | ||
| No psychological stress (no concern) | Psychological stress (requires concern) | |
| Scores | Score 2 or less than 2 | Score 3 or above |
| Total members | 23 (32%) | 49 (68%) |
As a communicable disease, and now a global Public Health Emergency (PHE), COVID-19 places a unique challenge on our health and social care workforce that will disrupt not just their usual work duties but also their social context [9]. Worldwide, COVID-19 has affected large numbers of frontline HCWs. As of March 2020, COVID-19 has infected more than 3000 HCWs in China only [10]. However, since the COVID-19 outbreak, the laboratory management system has become particularly vulnerable. The Most prominent issue is that a tremendous burden is placed on clinical laboratory resources. Generally, Because of cost containment strategies and laboratory space size, clinical laboratories have been designed and organized to sustain a customized volume of tests for a local health system, rather than concerned with rapidly expanding their testing capabilities [6,11]. Unfortunately, as COVID-19 continues to spread, the daily activity in separate clinical laboratories is rapidly saturated or even overwhelmed and disrupted by the large numbers of tests for COVID- 19 [12-14].
During outbreaks, the HCWs experience considerable stress. HCW’S reported extreme somatization, depression, anxiety, and obsession-compulsion. Risk factors for mental health include overwhelming situations, social disruption of daily life, feeling vulnerable, at risk of getting infected, fear of transmitting the disease to families, and loved ones [15,16]. The majority of studies focused on the psychological impact of COVID-19 on frontline HCW’s whereas none of the studies in the literature talked about the impact of COVID-19 on laboratory health workers. This review suggested how laboratory health workers’ life is impacted by COVID-19 preferably in both the view including physically and mentally. Our study found that the female gender had a significantly higher risk of psychological stress which is following the published data during epidemics where a female working in a healthcare system was more prone to develop depression and anxiety [3.17,18]. Our study shows that respondents with higher age (30 years - 50 years) have a significantly higher impact on mental health. This might be due to higher mortality risk among the elderly population and older adults are committing suicide due to a relapse of a depressive illness during the COVID-19 outbreak. These results were concordant with other studies [14,19,20]. Most of the laboratory staff workers were using social media to cope with their mental health issues followed by the use of psychological aids in the form of books. Similarly, only 4% of respondents used psychotherapy or counseling to win the battle against psychological problems during the COVID-19 outbreak [21-23]. The study found that laboratory workers experienced anxiety about their own and their family’s safety (along with their patients) but maintained the professional obligation to effectively complete their work. Like our study, many studies have been conducted that have detected the presence of depression and anxiety among HCWs [24-26]. Sun, et al. results indicated that in the early stages of the outbreak, anxiety and fear were prevalent which led to feelings of helplessness. The authors noted some healthy coping strategies, including team encouragement and rational thinking [27]. Routine management inside the separate laboratories could not cater to the demand of the COVID-19 public health emergency [28,29]. Public health emergencies impacting the laboratory medicine discipline, and the management of laboratory medicine faced many challenges [30-33]. The authors found that older staff had increased stress related to increased risk of infection, (lack of) PPE, and longer work hours which further exacerbated the existing shortage of skilled workforce [34-37]. Literature found that Battling COVID-19 on the frontline makes lab staff vulnerable to psychological distress including high levels of depression, stress, anxiety, distress, anger, fear, insomnia, and post-traumatic stress disorder [38-40]. The study found that the female gender predicted a greater risk of psychological stress including depression, anxiety, insomnia, and distress which is similar to the other studies. Coping strategies used by laboratory staff workers included adhering to strict protective measures, following isolation guidelines, and exhibiting a positive mindset [41].
Laboratory professionals also continue to suffer from unprecedented challenges and fears. The financial implications, the declining motivation levels, inadequate provision of PPE harnessing safety concerns, the additional stress of transport arrangement during the lockdown, and the fear of being laid off from the job amid the COVID-19 crisis are major concerns requiring immediate attention by the management, as they can potentially affect efficiency and productivity.
- Cabarkapa S, Nadjidai SE, Murgier J, Ng CH. The psychological impact of COVID-19 and other viral epidemics on frontline healthcare workers and ways to address it: A rapid systematic review. Brain Behav Immun Health. 2020 Oct;8:100144. doi: 10.1016/j.bbih.2020.100144. Epub 2020 Sep 17. PMID: 32959031; PMCID: PMC7494453.
- Shaukat N, Ali DM, Razzak J. Physical and mental health impacts of COVID-19 on healthcare workers: a scoping review. Int J Emerg Med. 2020 Jul 20;13(1):40. doi: 10.1186/s12245-020-00299-5. PMID: 32689925; PMCID: PMC7370263.
- Hayat K, Arshed M, Fiaz I, Afreen U, Khan FU, Khan TA, Kadirhaz M, Shukar S, Saeed A, Gill MR, Fang Y. Impact of COVID-19 on the Mental Health of Healthcare Workers: A Cross-Sectional Study From Pakistan. Front Public Health. 2021 Apr 26;9:603602. doi: 10.3389/fpubh.2021.603602. PMID: 33981657; PMCID: PMC8107369.
- Andrew B, Robert B, Chee H. L. Impact of the COVID-19 pandemic –a mental health service perspective. 2021; 25 (2): 27-33
- Muller AE, Hafstad EV, Himmels JPW, Smedslund G, Flottorp S, Stensland SØ, Stroobants S, Van de Velde S, Vist GE. The mental health impact of the covid-19 pandemic on healthcare workers, and interventions to help them: A rapid systematic review. Psychiatry Res. 2020 Nov;293:113441. doi: 10.1016/j.psychres.2020.113441. Epub 2020 Sep 1. PMID: 32898840; PMCID: PMC7462563.
- Lippi G, Plebani M. The critical role of laboratory medicine during coronavirus disease 2019 (COVID-19) and other viral outbreaks. Clin Chem Lab Med. 2020 Jun 25;58(7):1063-1069. doi: 10.1515/cclm-2020-0240. PMID: 32191623.
- Lippi G, Plebani M. Laboratory medicine resilience during coronavirus disease 2019 (COVID-19) pandemic. Adv Lab Med. 2020 Apr 21;1(2):20200035. doi: 10.1515/almed-2020-0035. PMID: 37363774; PMCID: PMC10158742.
- Mitra P, Misra S, Sharma P. Impact of COVID-19 on Clinical Biochemistry: Indian Scenario. Indian J Clin Biochem. 2021 Oct;36(4):385-386. doi: 10.1007/s12291-021-01003-x. Epub 2021 Sep 6. PMID: 34511753; PMCID: PMC8419656.
- Markwell A, Mitchell R, Wright AL, Brown AF. Clinical and ethical challenges for emergency departments during communicable disease outbreaks: Can lessons from Ebola Virus Disease be applied to the COVID-19 pandemic? Emerg Med Australas. 2020 Jun;32(3):520-524. doi: 10.1111/1742-6723.13514. Epub 2020 May 5. PMID: 32275805; PMCID: PMC7262026.
- Remuzzi A, Remuzzi G. COVID-19 and Italy: what next? Lancet. 2020 Apr 11;395(10231):1225-1228. doi: 10.1016/S0140-6736(20)30627-9. Epub 2020 Mar 13. PMID: 32178769; PMCID: PMC7102589.
- Alamoodi AH, Zaidan BB, Zaidan AA, Albahri OS, Mohammed KI, Malik RQ, Almahdi EM, Chyad MA, Tareq Z, Albahri AS, Hameed H, Alaa M. Sentiment analysis and its applications in fighting COVID-19 and infectious diseases: A systematic review. Expert Syst Appl. 2021 Apr 1;167:114155. doi: 10.1016/j.eswa.2020.114155. Epub 2020 Oct 28. PMID: 33139966; PMCID: PMC7591875.
- Ji D, Ji YJ, Duan XZ, Li WG, Sun ZQ, Song XA, Meng YH, Tang HM, Chu F, Niu XX, Chen GF, Li J, Duan HJ. Prevalence of psychological symptoms among Ebola survivors and healthcare workers during the 2014-2015 Ebola outbreak in Sierra Leone: a cross-sectional study. Oncotarget. 2017 Feb 21;8(8):12784-12791. doi: 10.18632/oncotarget.14498. PMID: 28061463; PMCID: PMC5355054.
- Koh D. Occupational risks for COVID-19 infection. Occup Med (Lond). 2020 Mar 12;70(1):3-5. doi: 10.1093/occmed/kqaa036. PMID: 32107548; PMCID: PMC7107962.
- Rana U. Elderly suicides in India: an emerging concern during COVID-19 pandemic. Int Psychogeriatr. 2020 Oct;32(10):1251-1252. doi: 10.1017/S1041610220001052. Epub 2020 Jun 3. PMID: 32487275; PMCID: PMC7322164.
- Luo Y, Wang J, Zhang M, Wang Q, Chen R, Wang X, Wang H. COVID-19-another influential event impacts on laboratory medicine management. J Clin Lab Anal. 2021 Jun;35(6):e23804. doi: 10.1002/jcla.23804. Epub 2021 May 25. PMID: 34032325; PMCID: PMC8183907.
- De Kock JH, Latham HA, Leslie SJ, Grindle M, Munoz SA, Ellis L, Polson R, O'Malley CM. A rapid review of the impact of COVID-19 on the mental health of healthcare workers: implications for supporting psychological well-being. BMC Public Health. 2021 Jan 9;21(1):104. doi: 10.1186/s12889-020-10070-3. PMID: 33422039; PMCID: PMC7794640.
- Yang JY, Parkins MD, Canakis A, Aroniadis OC, Yadav D, Dixon RE, Elmunzer BJ, Forbes N; DMC-19 Study Group and the North American Alliance for the Study of Digestive Manifestations of COVID-19. Outcomes of COVID-19 Among Hospitalized Health Care Workers in North America. JAMA Netw Open. 2021 Jan 4;4(1):e2035699. doi: 10.1001/jamanetworkopen.2020.35699. PMID: 33507259; PMCID: PMC7844592.
- Shreffler J, Petrey J, Huecker M. The Impact of COVID-19 on Healthcare Worker Wellness: A Scoping Review. West J Emerg Med. 2020 Aug 17;21(5):1059-1066. doi: 10.5811/westjem.2020.7.48684. PMID: 32970555; PMCID: PMC7514392.
- Mehta S, Machado F, Kwizera A, Papazian L, Moss M, Azoulay É, Herridge M. COVID-19: a heavy toll on health-care workers. Lancet Respir Med. 2021 Mar;9(3):226-228. doi: 10.1016/S2213-2600(21)00068-0. Epub 2021 Feb 5. PMID: 33556317; PMCID: PMC7906726.
- Al Dhaheri AS, Bataineh MF, Mohamad MN, Ajab A, Al Marzouqi A, Jarrar AH, Habib-Mourad C, Abu Jamous DO, Ali HI, Al Sabbah H, Hasan H, Stojanovska L, Hashim M, Abd Elhameed OA, Shaker Obaid RR, ElFeky S, Saleh ST, Osaili TM, Cheikh Ismail L. Impact of COVID-19 on mental health and quality of life: Is there any effect? A cross-sectional study of the MENA region. PLoS One. 2021 Mar 25;16(3):e0249107. doi: 10.1371/journal.pone.0249107. PMID: 33765015; PMCID: PMC7993788.
- Tang YW, Schmitz JE, Persing DH, Stratton CW. Laboratory Diagnosis of COVID-19: Current Issues and Challenges. J Clin Microbiol. 2020 May 26;58(6):e00512-20. doi: 10.1128/JCM.00512-20. PMID: 32245835; PMCID: PMC7269383.
- Jafri L, Ahmed S, Siddiqui I. Impact of COVID-19 on laboratory professionals-A descriptive cross sectional survey at a clinical chemistry laboratory in a developing country. Ann Med Surg (Lond). 2020 Jul 18;57:70-75. doi: 10.1016/j.amsu.2020.07.022. PMID: 32704368; PMCID: PMC7367796.
- Santarone K, McKenney M, Elkbuli A. Preserving mental health and resilience in frontline healthcare workers during COVID-19. Am J Emerg Med. 2020 Jul;38(7):1530-1531. doi: 10.1016/j.ajem.2020.04.030. Epub 2020 Apr 15. PMID: 32336584; PMCID: PMC7156943.
- Penwell-Waines L, Ward W, Kirkpatrick H, Smith P, Abouljoud M. Perspectives on Healthcare Provider Well-Being: Looking Back, Moving Forward. J Clin Psychol Med Settings. 2018 Sep;25(3):295-304. doi: 10.1007/s10880-018-9541-3. PMID: 29536320.
- O'Dowd E, O'Connor P, Lydon S, Mongan O, Connolly F, Diskin C, McLoughlin A, Rabbitt L, McVicker L, Reid-McDermott B, Byrne D. Stress, coping, and psychological resilience among physicians. BMC Health Serv Res. 2018 Sep 21;18(1):730. doi: 10.1186/s12913-018-3541-8. PMID: 30241524; PMCID: PMC6151040.
- Nanda A, Wasan A, Sussman J. Provider Health and Wellness. J Allergy Clin Immunol Pract. 2017 Nov-Dec;5(6):1543-1548. doi: 10.1016/j.jaip.2017.05.025. Epub 2017 Jul 19. PMID: 28734859.
- Sun N, Wei L, Shi S, Jiao D, Song R, Ma L, Wang H, Wang C, Wang Z, You Y, Liu S, Wang H. A qualitative study on the psychological experience of caregivers of COVID-19 patients. Am J Infect Control. 2020 Jun;48(6):592-598. doi: 10.1016/j.ajic.2020.03.018. Epub 2020 Apr 8. PMID: 32334904; PMCID: PMC7141468.
- Lu W, Wang H, Lin Y, Li L. Psychological status of medical workforce during the COVID-19 pandemic: A cross-sectional study. Psychiatry Res. 2020 Jun;288:112936. doi: 10.1016/j.psychres.2020.112936. Epub 2020 Apr 4. PMID: 32276196; PMCID: PMC7195354.
- Li Z, Ge J, Yang M, Feng J, Qiao M, Jiang R, Bi J, Zhan G, Xu X, Wang L, Zhou Q, Zhou C, Pan Y, Liu S, Zhang H, Yang J, Zhu B, Hu Y, Hashimoto K, Jia Y, Wang H, Wang R, Liu C, Yang C. Vicarious traumatization in the general public, members, and non-members of medical teams aiding in COVID-19 control. Brain Behav Immun. 2020 Aug;88:916-919. doi: 10.1016/j.bbi.2020.03.007. Epub 2020 Mar 10. PMID: 32169498; PMCID: PMC7102670.
- Naser Moghadasi A. Evaluation of the Level of Anxiety among Iranian Multiple Sclerosis Fellowships During the Outbreak of COVID-19. Arch Iran Med. 2020 Apr 1;23(4):283. doi: 10.34172/aim.2020.13. PMID: 32271605.
- Zhang WR, Wang K, Yin L, Zhao WF, Xue Q, Peng M, Min BQ, Tian Q, Leng HX, Du JL, Chang H, Yang Y, Li W, Shangguan FF, Yan TY, Dong HQ, Han Y, Wang YP, Cosci F, Wang HX. Mental Health and Psychosocial Problems of Medical Health Workers during the COVID-19 Epidemic in China. Psychother Psychosom. 2020;89(4):242-250. doi: 10.1159/000507639. Epub 2020 Apr 9. PMID: 32272480; PMCID: PMC7206349.
- Liu CY, Yang YZ, Zhang XM, Xu X, Dou QL, Zhang WW, Cheng ASK. The prevalence and influencing factors in anxiety in medical workers fighting COVID-19 in China: a cross-sectional survey. Epidemiol Infect. 2020 May 20;148:e98. doi: 10.1017/S0950268820001107. PMID: 32430088; PMCID: PMC7251286.
- Jin YH, Huang Q, Wang YY, Zeng XT, Luo LS, Pan ZY, Yuan YF, Chen ZM, Cheng ZS, Huang X, Wang N, Li BH, Zi H, Zhao MJ, Ma LL, Deng T, Wang Y, Wang XH. Perceived infection transmission routes, infection control practices, psychosocial changes, and management of COVID-19 infected healthcare workers in a tertiary acute care hospital in Wuhan: a cross-sectional survey. Mil Med Res. 2020 May 11;7(1):24. doi: 10.1186/s40779-020-00254-8. PMID: 32393381; PMCID: PMC7211983.
- Ehrlich H, McKenney M, Elkbuli A. Protecting our healthcare workers during the COVID-19 pandemic. Am J Emerg Med. 2020 Jul;38(7):1527-1528. doi: 10.1016/j.ajem.2020.04.024. Epub 2020 Apr 17. PMID: 32336585; PMCID: PMC7162741.
- Chan-Yeung M. Severe acute respiratory syndrome (SARS) and healthcare workers. Int J Occup Environ Health. 2004 Oct-Dec;10(4):421-7. doi: 10.1179/oeh.2004.10.4.421. PMID: 15702757.
- Evans DK, Goldstein M, Popova A. Health-care worker mortality and the legacy of the Ebola epidemic. Lancet Glob Health. 2015 Aug;3(8):e439-e440. doi: 10.1016/S2214-109X(15)00065-0. Epub 2015 Jul 9. PMID: 26163833.
- Abolfotouh MA, AlQarni AA, Al-Ghamdi SM, Salam M, Al-Assiri MH, Balkhy HH. An assessment of the level of concern among hospital-based health-care workers regarding MERS outbreaks in Saudi Arabia. BMC Infect Dis. 2017 Jan 3;17(1):4. doi: 10.1186/s12879-016-2096-8. PMID: 28049440; PMCID: PMC5210292.
- Wang J, Zhou M, Liu F. Reasons for healthcare workers becoming infected with novel coronavirus disease 2019 (COVID-19) in China. J Hosp Infect. 2020 May;105(1):100-101. doi: 10.1016/j.jhin.2020.03.002. Epub 2020 Mar 6. PMID: 32147406; PMCID: PMC7134479.
- Kang L, Li Y, Hu S, Chen M, Yang C, Yang BX, Wang Y, Hu J, Lai J, Ma X, Chen J, Guan L, Wang G, Ma H, Liu Z. The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. Lancet Psychiatry. 2020 Mar;7(3):e14. doi: 10.1016/S2215-0366(20)30047-X. Epub 2020 Feb 5. PMID: 32035030; PMCID: PMC7129673.
- Nguyen LH, Drew DA, Graham MS, Joshi AD, Guo CG, Ma W, Mehta RS, Warner ET, Sikavi DR, Lo CH, Kwon S, Song M, Mucci LA, Stampfer MJ, Willett WC, Eliassen AH, Hart JE, Chavarro JE, Rich-Edwards JW, Davies R, Capdevila J, Lee KA, Lochlainn MN, Varsavsky T, Sudre CH, Cardoso MJ, Wolf J, Spector TD, Ourselin S, Steves CJ, Chan AT; COronavirus Pandemic Epidemiology Consortium. Risk of COVID-19 among front-line health-care workers and the general community: a prospective cohort study. Lancet Public Health. 2020 Sep;5(9):e475-e483. doi: 10.1016/S2468-2667(20)30164-X. Epub 2020 Jul 31. PMID: 32745512; PMCID: PMC7491202.
- Mani NS, Budak JZ, Lan KF, Bryson-Cahn C, Zelikoff A, Barker GEC, Grant CW, Hart K, Barbee CJ, Sandoval MD, Dostal CL, Corcorran M, Ungerleider HM, Gates JO, Olin SV, Bryan A, Hoffman NG, Marquis SR, Harvey ML, Nasenbeny K, Mertens K, Chew LD, Greninger AL, Jerome KR, Pottinger PS, Dellit TH, Liu C, Pergam SA, Neme S, Lynch JB, Kim HN, Cohen SA. Prevalence of Coronavirus Disease 2019 Infection and Outcomes Among Symptomatic Healthcare Workers in Seattle, Washington. Clin Infect Dis. 2020 Dec 17;71(10):2702-2707. doi: 10.1093/cid/ciaa761. PMID: 32548613; PMCID: PMC7337651.